Strain elastography does not have additional benefits over conventional elastography-guided fine-needle aspiration cytology (FNAC) for diagnosing malignancy in thyroid nodules, suggest findings published October 15 in Radiology.
A team led by Hisham Mehanna, PhD, from the University of Birmingham in England, found that strain ultrasound elastography does not reduce the nondiagnostic rate of FNAC, as well as the number of thyroidectomies or unnecessary thyroidectomies performed.
“Reporting a positive experience with ultrasound elastography and having higher case throughputs did not result in the radiologist having better ultrasound elastography outcomes,” the Mehanna team wrote.
Ultrasound-guided FNAC is the conventional technique used for diagnosing malignant thyroid nodules, but it has its flaws, including having a nondiagnostic rate of up to 20%. Previous studies suggest that strain elastography holds promise in improving thyroid nodule diagnosis, but Mehanna and colleagues noted that these studies are small and underpowered. They added that to their knowledge, no study has directly compared the performance of strain elastography and ultrasound-guided FNAC.
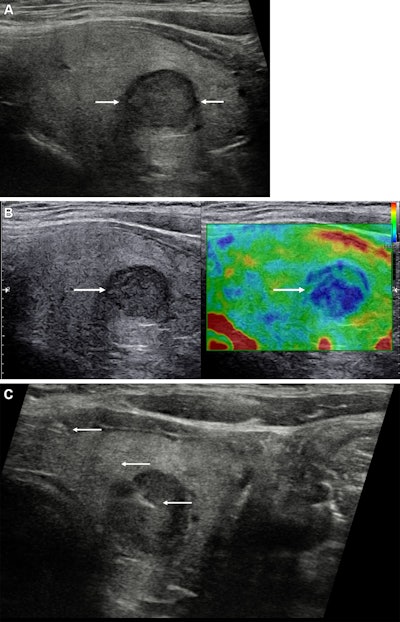
Images depict a 43-year-old woman with a solitary left-sided thyroid nodule classified at gray-scale ultrasound as category U3, upgraded to category U4 at strain elastography, and classified as category Thy4 at cytopathologic examination. Subsequent surgical histopathologic examination confirmed papillary cell carcinoma. (A) Longitudinal view of the left thyroid lobe demonstrates the low reflective nodule (between arrows) measuring 13 × 12 × 11 mm (not shown) and with a halo. (B) A longitudinal image with side-by-side visualization of the nodule (arrow) at gray scale (left) and strain elastography (right). The nodule is predominantly blue, indicating increased stiffness. (C) A longitudinal view shows the needle (arrows) within the stiffer aspect of the nodule for cytology sampling. U and Thy categories are according to British Thyroid Association system. Image courtesy of the RSNA.
The researchers did just that in their multicenter randomized controlled trial, which was performed at 18 secondary and tertiary hospitals across England between 2015 and 2018.
The final analysis included data from 982 participants with single or multiple thyroid nodules who had not previously undergone FNAC. The participants were randomized to the elastography FNAC group (n = 493) or the conventional ultrasound FNAC group (n = 489). Of the 493 participants who underwent elastography, 467 were examined with strain elastography.
The researchers found no significant differences in the nondiagnostic rate or malignancy rate between the two groups.
Performance of elastography-, ultrasound-guided FNAC Measure Ultrasound FNAC Elastography FNAC p-value Nondiagnostic rate 16% 19% 0.11 Malignancy rate 16% 4% 0.39 Rate of undergoing hemi-thyroidectomy 40% 37% 0.15The team also found no significant difference in the median time to reach the final definitive diagnosis, 3.3 months for elastography FNAC and 3.4 months for ultrasound FNAC.
Finally, neither group showed any advantage over the other in the rate of benign histologic findings between the groups (risk difference, −0.01; p = 0.7).
While the trial found no benefit from choosing strain elastography over conventional ultrasound FNAC in this area, new developments could make way for elastography, the study authors wrote. These include carotid pulsation replacing manual compression and elastography techniques becoming more automated and standardized.
“Coupled with better data processing, more accurate color mapping, and AI assessment of parameters, these changes may improve the efficacy of ultrasound elastography in the future but would require rigorous assessment before clinical rollout,” the authors added.
Future research on elastography’s utility in this area would be beneficial, according to an accompanying editorial written by Masis Isikbay, MD, and Joelle Harwin, MD, both from the University of California, San Francisco. They added that there are many areas of study in addition to TI-RADS that could aid in risk stratification.
“Further exploration of thyroid nodule growth kinetics could provide valuable information relevant to the risk stratification of these lesions,” Isikbay and Harwin wrote. “With advancements in machine learning, automated growth calculators, and the use of large institutional patient datasets, this work could become feasible.”
The full results can be found here.
Whether you are a professional looking for a new job or a representative of an organization who needs workforce solutions - we are here to help.